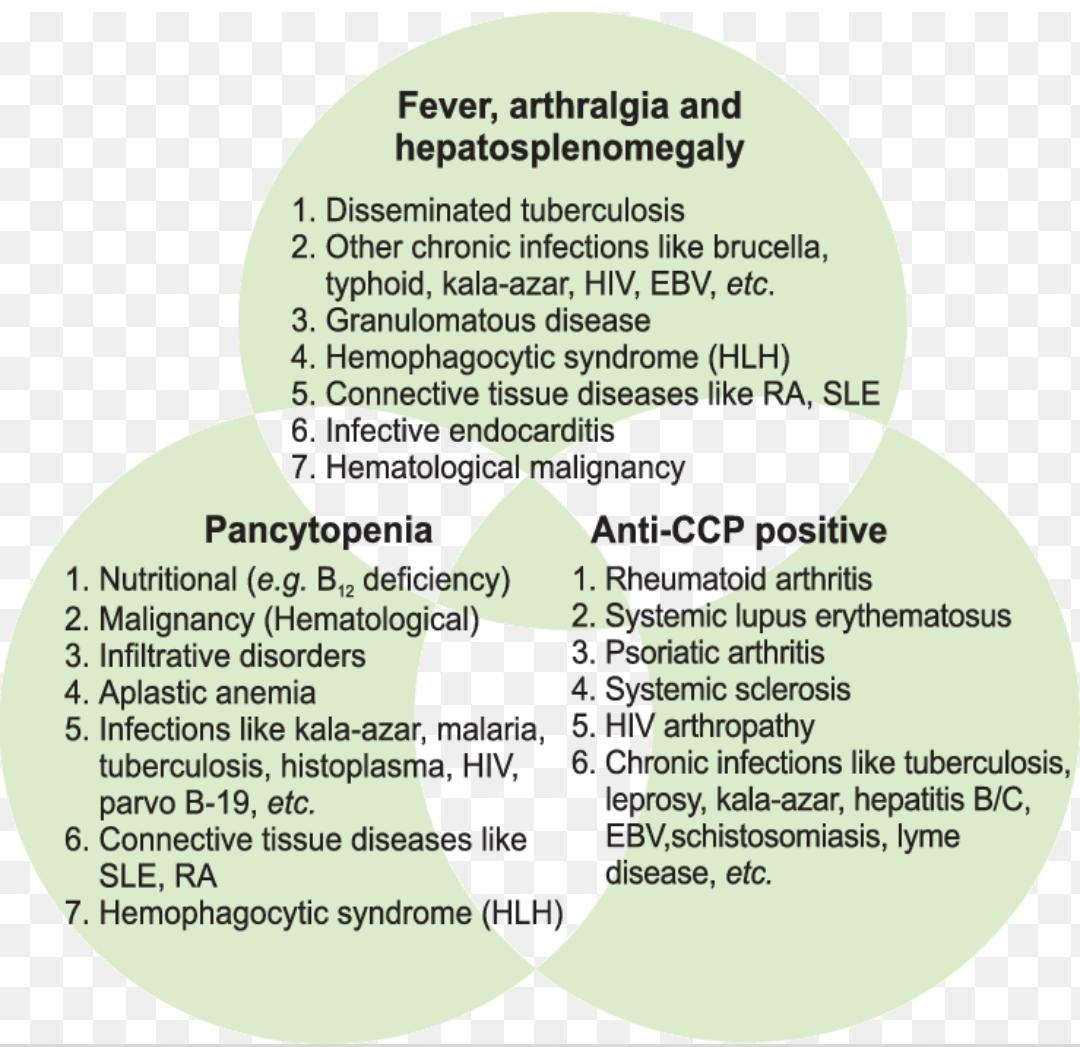
dimorphic anemia with hyponatremia
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen
52 year old male , shopkeeper by profession complains of SOB, cough ,decrease sleep and appetite since 10 days .
patient was apparently asymptomatic 10 days back then he developed sob ( grade 2 _3) according to NYHA classification, no complains of palpitations , chest pain ,orthopnea and pnd
Complains of
cough with sputum. whitish in colour non foul smelling since 2 days
Complains of decreased sleep since 10 days.
Same history approximately a year back for which he went to near by rmp and started using tablets ( vitamins) since then
No history of melena ,palpitations,pedal edema,burning micturition ,wt loss,night sweats
Known case of DM ans HTN
using teneligliptin 20mg and Telmisartan + metoprolol succinate for the same. 9
purely vegetarian.. occasionally non vegetarian
Non alcoholic
non smoker
General examination
Patient is conscious ,coherent ,coopertive
Moderately built and nourished
Pallor is present
No icterus ,clubbing ,cyanosis,generalised edema and lymphadenopathy
Respiratory examination
Bilateral air entry present , normal vesicular breath sounds , crepts present in the infrascapular region
CNS examination:
oriented to time place person he is alert conscious coherent cooperative ,
cranial nerves intact
Sensory and motor system examination is
normal
no signs of meningeal irritation
no cerebellar lesions
Cvs examination - pan systolic murmur heard
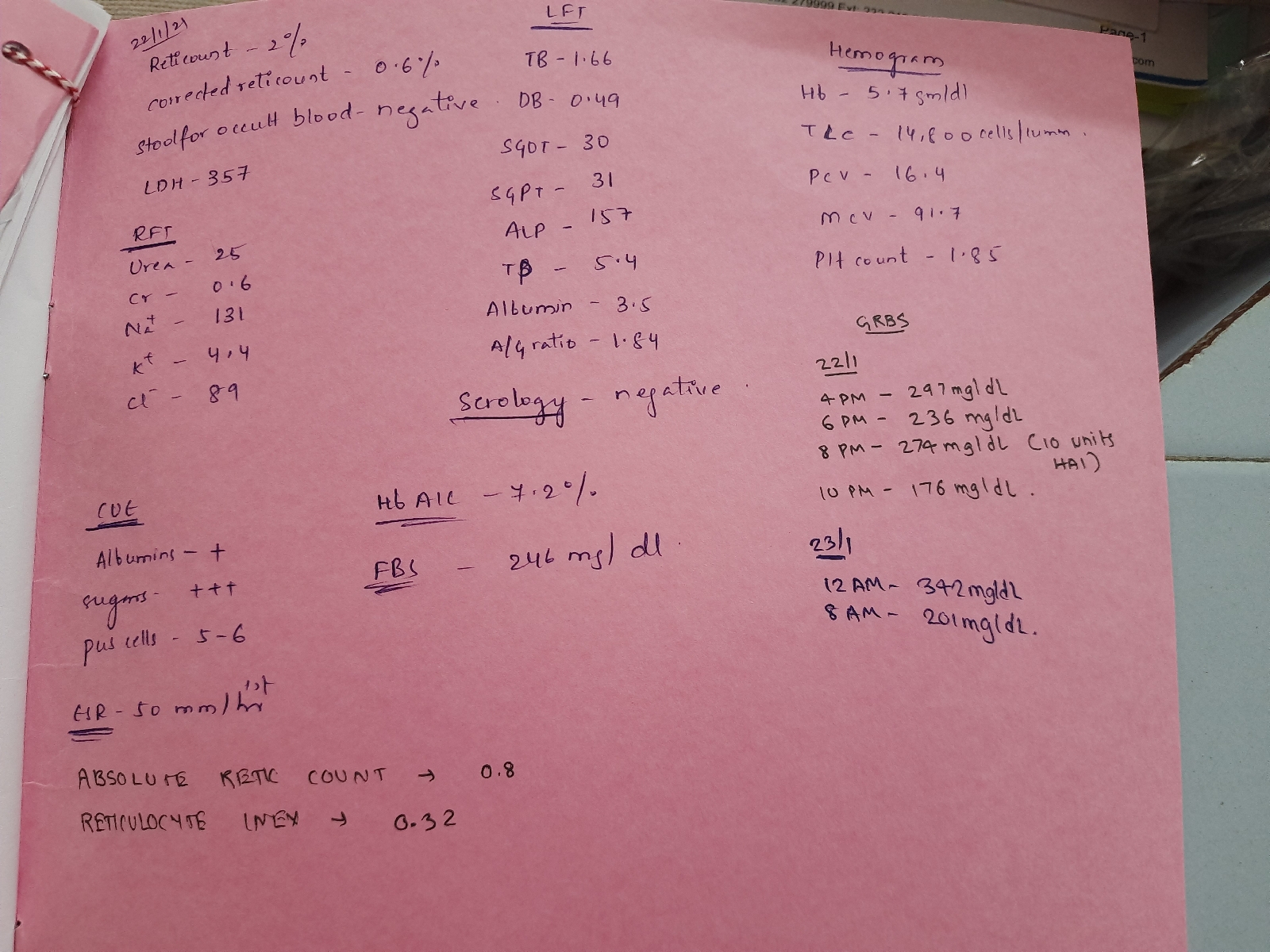
Na+ 127
K+ 3.0
Cl- 94
Tolvaptan given
.
On feb 1 st
Na + 139
K + 3.0
Cl- 98
10.GRBS PROFILE ( 7 POINT PROFILE ) MONITORING
Treatment at discharge
Inj Mixtard 25 units morning and evening SC
Inj H. Actrapid 16 units school
Tab Telma 40 mg PO/OD
Tab Metformin 500 mg Po/BD
Tab Toluvapton 7.5mg/PO/OD
Inj vit b 12 1000 mg /I'M/weekly once for 1 month
Tab folic acid 5 mg PO/OD for 1 week
T. Livogen 150 mg/PO/OD
The patient was completely fine all these days after the discharge with regular monitoring of blood sugars and receiving intra muscular injections of vitamin b12 and folic acid supplement s and orofer tablet to correct his dimorphic anemic status and carrying out his daily routine normal activities
And on 22 feb of this month he came to hospital with complaints of high blood sugars of around 400 mg/dl ( recorded via glucometer) on Friday and 509 mg/dl on Saturday despite using Anti diabetic drugs and presented/came in need of further evaluation of his high blood sugars.... No other complaints told by the patient
No history of fever, vomitings, loose stools, pain abdomen, pedal edema, shortness of breath, headache , fatigue, tinnitus
As already mentioned before, he is a known case of hypertension since 2 years and is on tablet telmisartan 40 mg plus amlodipine 5 mg and his hypertension is controlled. ..Not a known case of asthma, tb, epilepsy, CNS abnormalities
History of Dyselectrolemia(severe hyponatremia for which he received Toluvaptan for 1 week) which is resolved now, dimorphic anemia, nutritional anemia which still has to be corrected
No past surgical history
No history of blood transfusion
He is married, a rice business dealer, his appetite is normal, diet is pure vegetarian, bowel and bladder movement s r regular
Not an alcoholic nor smoker
Family history: no familial history of diabetes, hypertension, stroke, cancer, asthma, tuberculosistuberculosis
General examination:
Verbal consent of the patient is taken
Patient is conscious, oriented to time, place and person, coherent and cooperative
Pallor is present, no icterus, cyanosis, clubbing, generalised edema and lymphenopathy
Vitals at the time of admission:
BP:160/ 90
PR:96
RR:18
Spo2:99% @ RA
Temp:afebrile
Moderately built and nourished
CNS examination:
oriented to time place person he is alert conscious coherent cooperative ,
cranial nerves intact
Sensory and motor system examination is
normal
no signs of meningeal irritation
no cerebellar lesions
Respiratory system examination:
Bilateral air entry present, Non vesicular breath sounds heard, no wheeze and crepts
Per abdomen: soft , non tender , no organomegaly