bimonthly assessment february
1Q. 50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
a. What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
This was our unit case, and the first time I've seen a case with Progressive Supranuclear Palsy
50 year old man, detected to be a diabetic 9 months back, presented with the complaints of:
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
Bed wetting since 1 year
The patient also has had 3 suicidal attempts in the past.
He had reduced arm swing and facial apathy.
All of this fitting into a neurodegenerative disorder known as Progressive supranuclear palsy.
ANATOMICAL LOCALIZATION TO HIS PROBLEMS:
The anatomical localization to his problems appears to be in the brain
The anatomical location is in the Basal ganglia and substantia nigra
Goes in favour of a neurodegenrative disorder
The basal ganglia and the midbrain. In the midbrain, vertical and torsional saccades are controlled by the rostral interstitial medial longitudinal fasciculus (RIMLF).
'Isolated dysfunction of vertical eye movements is due to a midbrain lesion affecting the rostral interstitial nucleus of the medial longitudinal fascicle, with impaired vertical saccades only, the interstitial nucleus of Cajal or the posterior commissure; common causes with an acute onset are an infarction or bleeding in the upper midbrain or in patients with chronic progressive supranuclear palsy (PSP) and Niemann-Pick type C '
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
We came to a diagnosis that the patient probably has Progressive supranuclear palsy.
The other differential we had in mind was Myasthenia gravis as the patient complained of ptosis which progressed by the night. We performed an Ice Pack test to rule out Myasthenia Gravis. After an Ice pack test, in Myasthenia Gravis, the eyelid droop improves by atleast 2-3 mm, which wasn't seen in this patient & also the drooping of his eyelids were intermitted.
Upon examination, he found that he was unable to move his eyeballs upwards and he would frequently walk into objects and have frequent falls.
Postmortem autoradiographic studies indicate that pharmacologically defined D2 dopamine receptors are decreased in the striatum, but striatal D1 dopamine receptors are preserved. This situation contrasts with that found in Parkinson's disease, in which striatal dopamine loss is associated with normal or elevated numbers of striatal D2 receptors."
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 60 year old man with a history of CVA 6 months back presented with
Dyspnea since 2 months
Bilateral pedal edema since 2 months
Reduced urine output since 2 months
Generalised weakness since 2 months
His examination findings were Visible apical impulse, Pericardial bulge, visible pulsations, dilated veinsshift of apex beat to 6th ICS, Thrill at the apex, Loud S1 present, loud P2 present, S3 Accentuating on inspiration- RVS3, Expiration - LVS3
His Ecg shows poor R wave progression
Chest Xray PA shows Cardiomegaly
His 2Echo is suggestive of Heart failure DCMP with Hypokinesia at RCA, LCX
Anatomical diagnosis:
The location to his problems is at the Heart, secondary to atherosclerosis of the vessels
Risk factors:
Alcohol
Age of 60 years
Male gender
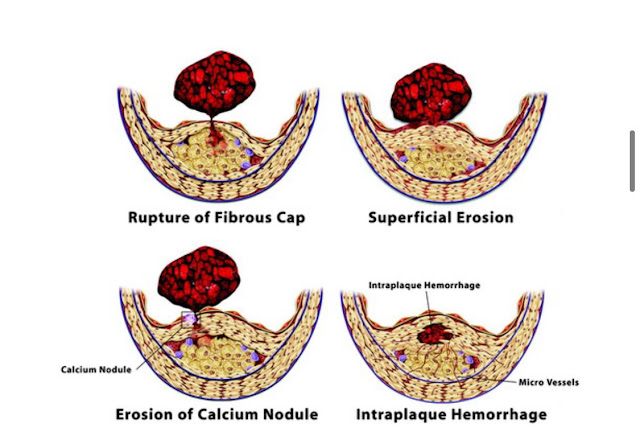
'In vivo imaging techniques applied in humans and the success of antithrombotic and fibrinolytic therapy in ACS established in practice the role of thrombosis in their pathogenesis. A number of microanatomic mechanisms underlie acute coronary thrombosis. According to autopsy studies—clearly biased toward fatal outcomes—a through-and-through rupture of the plaque’s protective fibrous cap most commonly causes lethal coronary thrombosis. Other mechanisms that account for a minority of fatal coronary thromboses include superficial erosion, intraplaque hemorrhage, and the erosion of a calcified nodule. Thus, physical disruption of the atherosclerotic plaque accounts for almost all acute coronary thromboses.'
'Disrupted plaques provoke thrombosis in several ways. First, contact with collagen in the plaque’s extracellular matrix can trigger platelet activation. Second, TF produced by macrophages and SMCs activates the coagulation cascade. The disrupted plaque thereby represents a “solid-state” stimulus to both thrombosis and coagulation; these pathways reinforce each other, as thrombin generation amplifies the activation of platelets and other cells in the lesion. Conversion of fibrinogen to fibrin and release of von Willebrand factor from activated platelets can provide the cross-linking molecular bridges between platelets that yield the dense, 3-dimensional network of platelets entrapped in fibrin characteristic of the “white” arterial thrombus
Etiology to his current problems :
CAD leading to DCMP
Diagnosis:
DCMP with an EF of 34% secondary to CAD
CVA 6 months back (? Left ischaemic stroke
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 52 year old man, who is a known to be a Diabetic and hypertensive presented with:
Dyspnea since 10 days
Productive cough since 2 days
Disturbed sleep since 10 days
Anatomical localization:
The anatomical location of the problem is in the lungs
Lower respiratory tract infection
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
No respiratory examination has been mentioned in the elog.
However his problems list are:
- Hyponatremia
-Lower respiratory tract infection
-Uncontrolled blood sugars
-Dimorphic Anemia
Unclear on the details of his ?UTI. CUE shows 5-6 pus cells, with no patients complaints with a negative urine culture & sensitivity report.
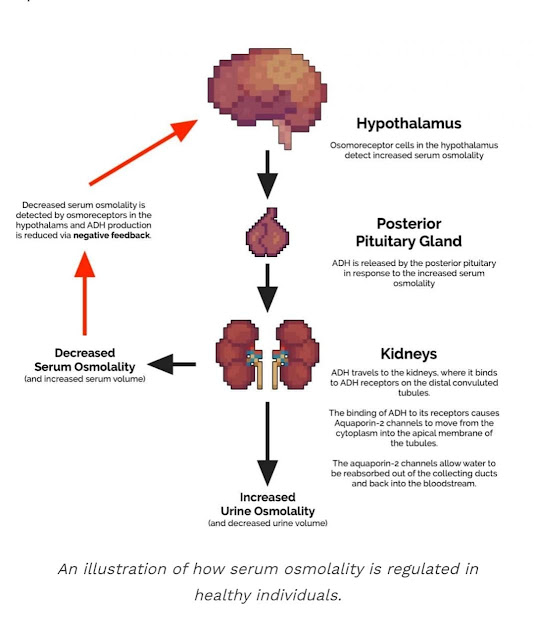
SIADH:
c) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient?
Randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of tolvaptan in Chinese patients with hyponatremia caused by SIADH
https://pubmed.ncbi.nlm.nih.gov/24906029/
P - 37 patients have been included in this study
I - Hyponatremic SIADH patients received tolvaptan (N = 19) at an initial dose of 15 mg/day with further titration to 30 mg/day and 60 mg/day based on serum sodium concentrations.
C - 18 patients received placebo
O -
Primary endpoint was the change of the serum sodium from baseline to days 4 and 7.
At day 4, average daily changes in serum sodium levels from baseline was 1.9 ± 2.9 mmol/L in the placebo group and 8.1 ± 3.6 mmol/L in the tolvaptan group; at day 7, the values were 2.5 ± 3.9 mmol/L and 8.6 ± 3.9 mmol/L for the placebo and tolvaptan groups
. At days 4 and 7, daily urine output and proportions of patients with normalized serum sodium were significantly superior in the tolvaptan group.
The most common adverse events occurring in the tolvaptan group were dry mouth and thirst. Tolvaptan demonstrated superiority to placebo in the treatment of Chinese SIADH patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4078649/
In this prospective observational study, data of 60 hospitalized patients having hyponatremia from February 2013 to July 2013 were collected and analyzed. Patients either received oral Tolvaptan or intravenous infusion of 3% hypertonic saline solution. The serum sodium concentration before administration of treatment and 24 h and 48 h after the administration of the drugs were recorded and analyzed.
Observation:
'Tolvaptan and 3% hypertonic saline solution had significant effects in raising serum sodium level in hyponatremic patients at both 24 h and 48 h (P < 0.0001). This increase was about 8.030 ± 0.6507 mEq/L and 12.33 ± 0.6489 mEq/L for 3% hypertonic saline and about 5.111 ± 0.6616 mEq/L and 10.11 ± 0.6230 mEq/L for Tolvaptan, after 24 h and 48 h, respectively
Both drugs had significant effects in raising serum sodium level in hyponatremic patients; however administration of 3% hypertonic saline solution had a slightly superior efficacy in raising the serum sodium concentration at both 24 h and 48 h periods in Hyponatremic patients compared with oral Tolvaptan.'
I don't think both Nacl and Tolvaptan could be given at the same time as there is a risk of overcorrection leading to hypernatremia.
4) Please mention your individual learning experiences from this month.